We're still struggling to understand whether infection with SARS-CoV-2, with or without COVID-19 symptoms, provides protection from further infections. Antibodies are an indicator of immunity and are the easiest aspect of the immune response to track. But data indicates that the generation of antibodies is highly variable, and their production may start fading within months. But there are many other aspects to the immune response, many of them centered on T cells. And here again, the response seems to be extremely complex.
Now, additional studies are coming out looking at other specialized aspects of the immune response. While these results provide some cause for optimism in terms of long-lasting immunity, there remain large numbers of unknowns.
Go with the flow
The two studies we'll look at were enabled by a technique called "flow cytometry" that has proven very useful for studying the immune response. It basically helps researchers get past the biggest issue with these studies: there's an abundance of very similar-looking cells involved in an immune response. While a trained eye can tell a T cell from a macrophage using a microscope, knowing there are T cells doesn't tell us much. Not only would we like to know how many of them there are, we'd need to know what types of T cells are present. T cells may help with the production of antibodies, they may kill infected cells, they might be used to remember exposure to pathogens, etc.
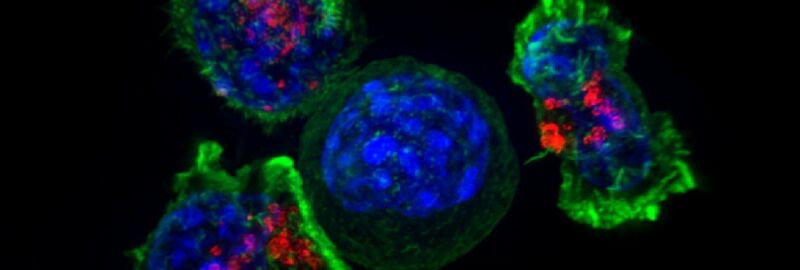
Flow cytometry can help tell us what cells are actually present. It involves taking the immune cells from a blood sample and getting them to flow past sensors one at a time. Each of these sensors can look at one aspect of the cell—typically, you label the cells with a fluorescent molecule that only sticks to specific cell types, and you use a laser to determine whether the molecule is present as a cell flows by. After the sensor, the device can redirect the flow to separate cells with and without these molecules.
So, if you make a fluorescent molecule that will stick to T cells, you can determine how many T cells are present and separate them all out. The key thing is that this can be done iteratively. Once you have the T cells, you can add another tag and separate out a single T cell population, like the killer T cells. And then you can separate out specific types of killer T cells from that population. Meanwhile, the other population—everything that's not a killer T cell—can also be sorted, allowing researchers to pull out the memory T cells, and so on.
This can give us a sense of which cells are present while an infection is ongoing. But not only that, its final output is a pure population of specialized cells, which can then be examined in more detail to try to figure out what they're up to.
Obviously, the more tags you can use to separate the cells, the more detailed your analysis can be. And, in this case, the researchers had access to equipment that could do a lot of separating: nearly 30 individual tags were used to separate out different cell populations. (Both papers have researchers from Sweden's Karolinska Institute, which is where this sophisticated bit of machinery is likely to reside.)
I remember this
In one paper, the research team focused on trying to find out which types of T cells are present in people infected by SARS-CoV-2 as well as what happens after the virus is cleared. Overall, the researchers had samples from over 200 people and data on their clinical outcomes—they knew which people had severe cases and could potentially correlate that with the presence of specific types of immune cells.
Those with active infections, it turned out, produced plenty of killer T cells, which target infected cells and eliminate them. The research team also found a difference after the infection had run its course. Here, those with symptoms, either mild or severe, seem to have produced a larger number of memory T cells, primed to fight off another SARS-CoV-2 infection.
The presence of these memory T cells was unrelated to whether the individual was producing antibodies to the virus, suggesting that they might serve as an alternate route to immune protection. Emphasis on the "might." The researchers emphasize that it "remains to be determined if robust memory T cell responses in the absence of detectable circulating antibodies can protect against severe forms of COVID-19." Also left in the "unknown" category is how long these memory cells will be retained—the answer is "over a decade" for SARS and MERS.
As in other recent studies, these researchers found that there were T cells poised to react to SARS-CoV-2 even in people who had never been exposed to it, possibly due to exposure to the coronaviruses that cause cold-like symptoms. Again, whether this provides any sort of protection is completely unclear.
More killers
T cells aren't the only ones that can kill infected cells; there's another type of blood cell, called a natural killer, that does so as well. While T cells are adaptive—they recognize a specific feature of one pathogen due to a unique receptor structure—natural killers broadly recognize cells infected by entire classes of pathogens. So, taking the same flow-cytometry equipment as was used in the other paper, a different research team analyzed what was going on with natural killers in a small population of patients with COVID-19 (both mild and severe cases).
Natural killer cells, as would be expected, had indications that they were activated by a SARS-CoV-2 infection, producing immune-signaling molecules and dividing to produce more of these cells. But there was little difference in this regard between those with mild and severe symptoms. There were, however, other differences that apparently did correlate with disease severity. Most notably, these include production of the protein that's used to kill infected cells, which is much more common in samples taken from patients with severe cases. Cells from those with severe cases also showed more indications of being involved in an inflammatory response.
By contrast, natural killer cells from people with mild COVID-19 symptoms tended to have high levels of what's called a "checkpoint" protein. These proteins help shut down the activity of cells unless certain conditions are met, and thus, might be involved with toning down the response of the natural killers.
Cause and effect
The challenge here, unfortunately, is separating cause and effect. It's not clear whether a more aggressive response by natural killer cells is producing the problems that come from an excessive inflammatory response and thus contributing to disease severity; it could just be that a more severe disease leads to a more aggressive natural killer response.
Overall, these two papers—and many more that continue to be published each week—are providing an ever more detailed look into the activity of the immune system in response to SARS-CoV-2. Unfortunately, the picture they're painting is extremely complex, and it doesn't neatly slot into any simple picture that could help with policy or treatments. T cells clearly maintain a memory of exposure to SARS-CoV-2, but it's not clear whether that's protective in the long run. Some immune cell types are more active in severe cases, but it's not clear whether we can identify this far enough in advance to tailor treatments.
Over time, a clearer picture will gradually emerge from the cumulative evidence that each of these studies is providing. But that will take time, and the likelihood that any single study will provide either a clear picture or a breakthrough is low.
Cell, 2020. DOI: 10.1016/j.cell.2020.08.017;
Science Immunology, 2020. DOI: 10.1126/sciimmunol.abd6832 (About DOIs).
reader comments
21